BES2024 BES 2024 CLINICAL CASE REPORTS (10 abstracts)
Hyperthyroidism unmasked: thinking beyond the thyroid
Pieter-Jan Martens 1 , Toon Van Gorp 2 , Jaak Billen 3 , Leen Antonio 4 & Marie Bex 1
1Department of Endocrinology. 2Department of Gynecologic Oncology. 3Department of Laboratory Medicine, University Hospitals Leuven, Leuven, Belgium
Introduction : Thyrotoxicosis is usually caused by an overproduction of thyroid hormones due to conditions such as Graves’ disease or thyroid nodules, or by an inflammation of the thyroid gland. We present a rare case in which both the pituitary and thyroid gland were intrinsically normal, yet endogenous severe hyperthyroidism ensued.
Case presentation: A 36-year-old female was referred by the gynecologist for evaluation of a worsening and unexplained thyrotoxicosis, diagnosed 11 weeks prior to her presentation to the emergency department with hematuria and urinary retention, caused by a pelvic mass. Her medical history is significant for endometriosis and a complete molar pregnancy, treated with two lines of chemotherapy (methotrexate and actinomycin D) eight years prior. Hormonal evaluation revealed a severe thyrotoxicosis (Table 1), previously not responding to a short course of thyrostatics (methimazole 30 mg daily) and later to therapy with corticosteroids (methylprednisolone 32 mg daily, tapered to 12 mg over 4 weeks). This treatment had been instituted as initially the presentation with a sore throat suggested a diagnosis of viral thyroiditis, especially in the absence of TSH-receptor and thyroid peroxidase antibodies and a normal thyroid ultrasound. Nevertheless, as her condition deteriorated, additional scintigraphic imaging revealed a homogenous high technetium uptake, which shifted the diagnosis back to antibody-negative Graves’ disease and methimazole was recommenced one week before referral. Further investigation identified the pelvic mass as malignant gestational trophoblastic disease (malignant GTD), characterized by high human chorionic gonadotropin (hCG) levels produced by syncytiotrophoblastic cells, that are monitored as key tumor marker to assess therapeutic efficacy. At high doses, hCG cross-reacts with the TSH receptor, causing hyperthyroidism with high isotope uptake, similar to Graves’. Initial hCG levels were only 6.769 IU/l, a level similar to those seen in the second month of pregnancy, but unexpectedly rose to >1.000.000 IU/l upon initiating chemotherapy. This paradoxical increase could be attributed to the “high-dose hook” effect, a phenomenon where extremely high analyte levels saturate both capture and detection antibodies in immunoassays, leading to falsely low or undetectable results. Diluting the prechemotherapy sample confirmed that hCG levels at diagnosis were much higher (hCG 2.883.000 IU/l). As chemotherapy progressed, hCG levels decreased, accompanied by an improvement in thyroid function and resolution of thyrotoxicosis (Table 1).
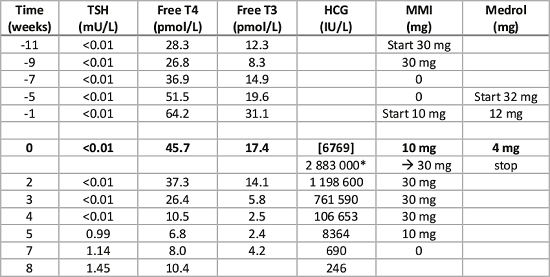
Table 1. Evolution of thyroid function tests over time (week 0 is at referral).
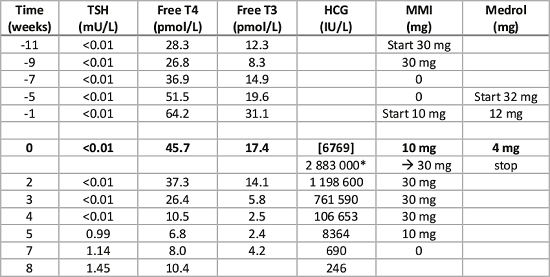
Conclusion: This case highlights the impact of hCG on thyroid function, attributable to its structural similarities to TSH, allowing hCG to weakly bind to TSH receptors and stimulate thyroid activity if present in high levels. Although rare, it might be worthwhile measuring hCG in cases of unexplained thyrotoxicosis. Furthermore, even when using current hCG immunoassays, in situations of clinically expected extremely elevated hCG levels, the high-dose hook effect must be considered, as it can lead to falsely low results. This phenomenon is critical to recognize when interpreting immunoassay results in similar clinical contexts.Table 1. Evolution of thyroid function tests over time (week 0 is at referral).As hCG levels decline, the thyroid function gradually improves so that ultimately methimazole can be discontinued while maintaining normalized thyroid function.Abbreviations: hCG: human chorionic gonadotropin. The initial undiluted hCG value (in parentheses) is affected by the high-dose hook effect; * same sample after dilution; Medrol: methylprednisolone; MMI: methimazole; T3: triiodothyronine (3.1-6.8); T4: thyroxine (11.9-21.6) ; TSH: thyroid-stimulating hormone (0.27-4.2).
 }
}



