BES2024 BES 2024 CLINICAL CASE REPORTS (10 abstracts)
Management of a mixed ACTH and prolactin secreting pituitary adenoma during pregnancy
Astrid Le Rigoleur 1 , Stefan Matei Constantinescu 1 , Martin Lammens 2,5 , Edward Fomekong 3 , Frédéric Debiève 4 , Dominique Maiter 5 & Orsalia Alexopoulou 1
1Department of Endocrinology and Nutrition. 2Neuropathology. 3Neurosurgery, and Obstetrics. 4Cliniques Universitaires Saint-Luc, Brussels, Belgium. 5Department of Pathology, Antwerp University Hospital, University of Antwerp, Antwerp, Belgium
Introduction : Mixed ACTH and prolactin secreting pituitary adenomas are extremely rare and can lead to both Cushing’s syndrome (CS), and galactorrhea and/or oligo-amenorrhea. No cases have ever been reported during pregnancy. Diagnosis of CS during pregnancy is challenging due to the physiological activation of the hypothalamic-pituitary-adrenal axis1, and it is associated with severe maternal and fetal complications1. Early diagnosis and treatment are therefore essential to improve feto-maternal outcomes. We describe the occurrence of a mixed pituitary macroadenoma secreting ACTH and prolactin successfully treated by transsphenoidal surgery (TSS) during pregnancy.
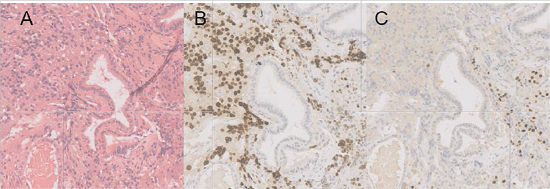
Case report: A 26-year-old woman was diagnosed with a centimetric prolactin secreting pituitary adenoma after developing oligomenorrhea, galactorrhea, and headaches. Hormonal data at diagnosis are not available. Cabergoline was initiated and up-titrated to 1.5 mg per week. Her menstrual cycles regularized but there was no improvement of galactorrhea. One year after cabergoline initiation, MRI showed no decrease in adenoma size, and blood tests revealed persistent hyperprolactinemia at 74.4 µg/l (normal 5.0 -23.0 µg/l) and increased ACTH at 143 pg/mL (normal 5.0 – 49.0 pg/mL). Concurrently, she gained weight, developed prediabetes and high blood pressure. The low-dose dexamethasone suppression test (0.5 mg every 6h for 48h) successfully suppressed plasma cortisol to 26.6 nmol/l and urinary free cortisol (UFC) was normal (34 µg/24h, normal<40µg/24h). Surgical management was suggested, but she did not have medical insurance and cabergoline was continued with close follow-up advised until administrative regularization. She was then lost to follow-up for over a year and was referred for the first time to our consultation because of an ongoing pregnancy and treatment resistant hypertension. She was 5 weeks pregnant, weighed 147 kg (BMI 52 kg/m2), and blood pressure was 150/90 mmHg. On clinical examination, she presented with fine abdominal stretch marks, buffalo neck, galactorrhea and lower limbs oedema. Blood tests at 5 weeks gestation showed hyperprolactinemia at 73.3µg/l. Morning cortisol was 417.4 mmol/l, afternoon cortisol was 369 nmol/l, ACTH was increased to 187.5 pg/mL and UFC was moderately elevated at 81,3 µg/24h, suggesting ACTH dependent hypercortisolism. A pituitary MRI at 12 weeks of pregnancy, revealed overall stability of the adenoma, which was in centre of the sella without cavernous sinus invasion. Given the risk of feto-maternal morbidity and mortality associated with CS, and after discussion at a multidisciplinary meeting for pituitary tumors, she underwent TSS at 16 weeks of pregnancy without any complications. The postoperative blood test showed normalization of prolactin and corticotropic insufficiency for which hydrocortisone was started. Pathological examination showed a single adenoma with positive staining for both PRL/PIT1 and ACTH/TPIT (Figure 1). Blood pressure rapidly normalized. We started insulin at 21 weeks of gestation for diabetes. A pituitary MRI at 27 weeks of pregnancy showed complete resection. A cesarean section was performed at 38 weeks and 6 days, after injection of 100 mg hydrocortisone IV, and a healthy boy of 3,25kg was born, with no maternal nor neonatal complications. Genetic testing is underway of inherited causes of pituitary adenomas.
Discussion: Only a few ACTH-PRL secreting adenomas have ever been reported 2.3. This association of hormones is unusual because of the different transcription factors necessary for the differentiation of lactotroph (PIT1 dependent) and corticotroph cells (TPIT dependent). Cabergoline therapy is an option in such cases and has been described to decrease both PRL and ACTH levels 2,3. This was not fully the case for our patient who showed resistance to cabergoline for both prolactin and ACTH. We hypothesize that the occurrence of pregnancy was possible because of the regularization of her menstrual cycles with cabergoline and because hypercortisolism was mild. This case highlights the importance of pre conceptional counselling and the safety and effectiveness of TSS for pregnant patients with Cushing’s disease.Figure 1: Pathological examinatio n showed a single adenoma with a m ixed PRL/PIT1 and ACTH/TPIT population. (A) Hematoxylin and eosin stain. (B) PIT1 staining. (C) TPIT staining. Immuno-histochemistry for prolactin and ACTH are not shown but matched the expected transcription factors
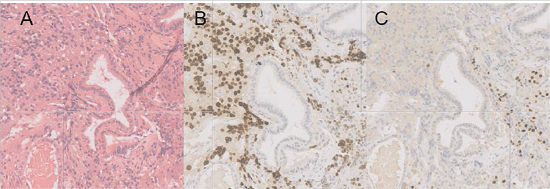
Figure 1: Pathological examination showed a single adenoma with a mixed PRL/PIT1 and ACTH/TPIT population. (A) Hematoxylin and eosin stain. (B) PIT1 staining. (C) TPIT staining. Immuno-histochemistry for prolactin and ACTH are not shown but matched the expected transcription factors
References
1. Hamblin R, Coulden A, Fountas A, Karavitaki N. The diagnosis and management of Cushing’s syndrome in pregnancy. J Neuroendocrinol 2022; 34(8): e13118.
2. T’Sjoen G, Defeyter I, Van De Saffele J, Rubens R, Vandeweghe M. Macroprolactinoma associatedwith Cushing’s disease, successfully treated with cabergoline. J Endocrinol Invest 2002; 25(2): 172-5.
3. Uraki S, Ariyasu H, Doi A, Furuta H, Nishi M, Usui T, Yamaue H, Akamizu T. Hypersecretion ofACTH and PRL from pituitary adenoma in MEN1, adequately managed by medical therapy. Endocrinol Diabetes Metab Case Rep. 2017 Apr 6;2017:17-0027.
 }
}



